| Australian College of Chiropractic Paediatrics |
Policy: Infant Hip Screening
JANUARY 2020
Note: This policy is relevant to infant ages only. A policy on hip screening in the post-infantile paediatric patient will be covered separately.
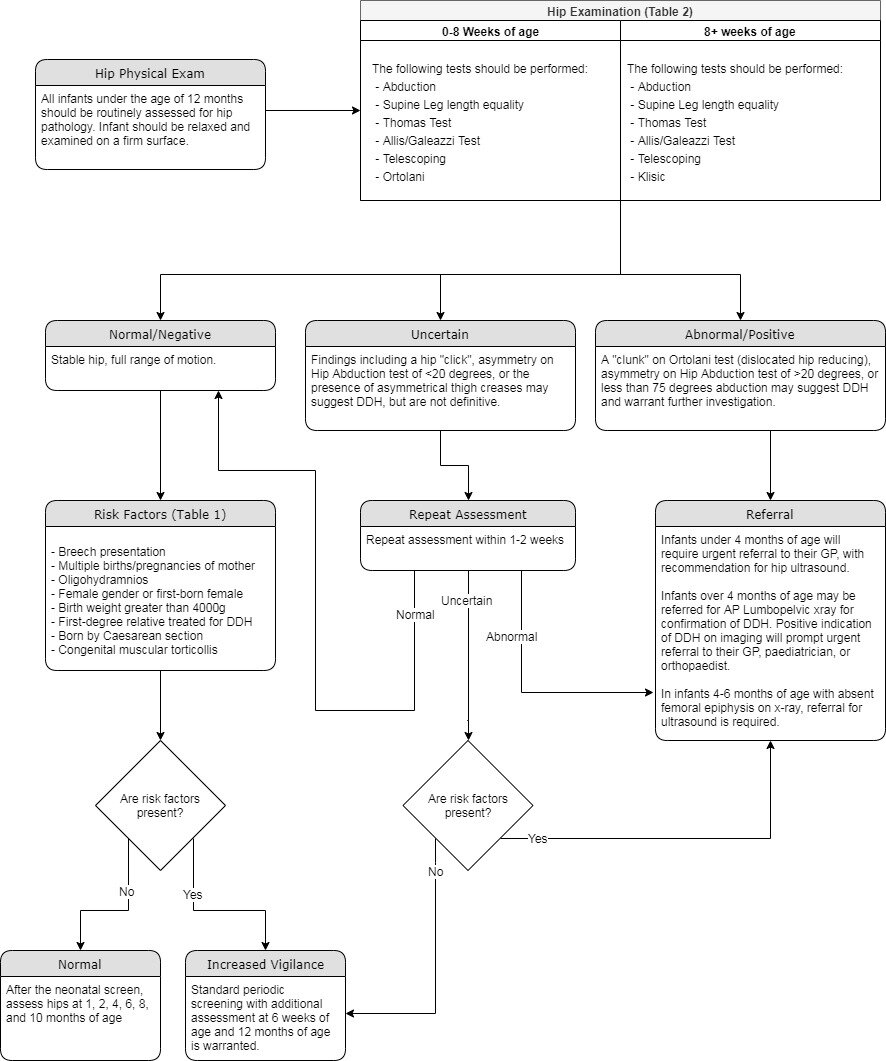
COMMITTEE ON CHIROPRACTIC PAEDIATRIC DIAGNOSTIC AND THERAPEUTIC PROCEDURESBACKGROUNDDevelopmental dysplasia of the hip (DDH) is one of the most common musculoskeletal conditions of infancy.(1) DDH is the result of abnormal relationship between the femoral head and the acetabulum. It can range in severity from instability to dislocation (requiring surgical intervention), with varying degrees of acetabular dysplasia in between.(2–4) In Australia, there is a reported incidence of seven per 1000 live births.(5) The incidence of late-detection (clinically detected DDH after 3 months of age) and diagnosis has increased from 0.22 per 1000 live births in 1988-2003 to 0.7 per 1000 in 2003-2009.(6,7) SCREENINGIn Australia, it is recommended that General Practitioners (GP) and Maternal and Child Health Nurses (MCHN) screen for DDH by performing Ortolani, Barlow, Abduction and Allis tests, as well as observing for leg length and thigh crease asymmetry.(8–11) This follows guidelines established by the American Academy of Orthopaedic Surgeons.(12) Regular screening is important as early detection of DDH has better outcomes and requires less aggressive management with reduced risks: bracing and non-surgical intervention compared to potential surgical intervention for those older than 6 months of age.(5) Clinical hip examination by the infants’ GP and MCHN remains the primary screening method to identify infants with possible DDH who require further investigation.(2,13–15) With appropriate training, non-medical staff such as chiropractors, physiotherapists and osteopaths, can be effectively used to conduct screening or surveillance utilising age-appropriate hip assessment tests.(16,17) The Hip Abduction test has high specificity (99.3%[18]) and negative predictive value (97.3%[18]) for unilateral DDH, making it ideal for screening in infants over 8 weeks of age,(2,14,15,18–20) however literature does stress the importance of compounding findings of multiple tests to reduce false negatives.(15,18–23) Age appropriate hip tests are detailed in Table 2. All non-ambulatory infants attending a chiropractor must undergo regular and routine hip assessment, even if recent assessment by another health practitioner has occurred. Frequency of assessment is modified according to the presence of risk factors. Chiropractors seeing infants should be aware of the risks factors for DDH (Table 1). In the infant without risk factors suggestive of DDH, after the neonatal screen it is recommended to assess hips at 4 and 8 weeks of age, as well as 4, 6, 8, and 10 months of age (MOA).(24) Additional screening at 6 weeks and 12MOA is appropriate particularly in the presence of risk factors suggestive of DDH. Consultation at these ages primarily for hip assessment is appropriate.
RISK FACTORSBreech Presentation (14,25) Limited hip abduction (25) Multiple births or pregnancies of mother (14,25) Born by Caesarean section (14) Oligohydramnios (14) Plagiocephaly* (26,27) Female gender/First-born female (14,25) Metatarsus Adductus* (28,29) Birth weight greater than 4000g (14) Congenital muscular torticollis* (25,26) First-Degree Relative treated for DDH/ Any family history of hip dysplasia (14) Increased frequency of assessment is appropriate in the presence of one or more risk factors, however risk factors alone are a poor predictor of DDH with only one in 75 infant with a risk factor having a dislocated hip.(30) Chiropractors should be aware that the risk factors for DDH change over time.(7,30,31) Risk factors for late-diagnosed DDH (DDH clinically detected after 3MOA) include rural birth, female gender, discharge from hospital within 4 days, and birthweight <2500g.(30) EXAMINATION0-8 WOA The following tests should be performed:
8WOA+ The following tests should be performed:
BILATERAL DDHBilateral DDH may be harder to detect clinically as there may be little asymmetry. Increased suspicion of the presence of bilateral DDH should be present in the following situations with early referral for imaging recommended. Findings suggestive of bilateral presentation DDH
DIAGNOSTIC IMAGINGIt is not recommended to refer for ultrasound at newborn screen.(24) Equivocal findings at the 4-week assessment with accompanying risk factors warrant referral for ultrasound.(24) Under 4 months of age Over 6 months of age Between 4 and 6 months of age REFERRALIn the presence of unequivocal positive findings on hip examination, referral for appropriate imaging is required (Figure 1). Figure 1 REFERENCES1. Gibson C, Scott H, Rice R, Scheil W. Birth Defects in South Australia 2013. Adelaide; 2017. 2. Sewell MD, Eastwood DM. Screening and treatment in developmental dysplasia of the hip-where do we go from here? Int Orthop. 2011;35(9):1359-1367. doi:10.1007/s00264-011-1257-z 3. Noordin S, Umer M, Hafeez K, Nawaz H. Developmental dysplasia of the hip. Orthop Rev (Pavia). 2010;2(e19):73-78. doi:10.4081/or.2010.e19 4. Shaw BA, Segal LS. Evaluation and Referral for Developmental Dysplasia of the Hip in Infants. Pediatrics. 2016;138(6):e1-e11. doi:10.1542/peds.2016-3107 5. Williams N. Improving early detection of developmental dysplasia of the hip through general practitioner assessment and surveillance. Aust J Gen Pract. 2018;47(9):615-619. 6. Williams N, Foster BK, Cundy PJ. Is swaddling damaging our babies’ hips? Med J Aust. 2012;197(5):272. doi:10.5694/mja12.10652 7. Studer K, Williams N, Antoniou G, et al. Increase in late diagnosed developmental dysplasia of the hip in South Australia: Risk factors, proposed solutions. Med J Aust. 2016;204(6):240.e1-240.e6. doi:10.5694/mja15.01082 8. Queensland Clinical Guidelines. Maternity and Neonatal Clinical Guideline: Routine Newborn Assessment. Queensland; 2014. www.health.qld.gov.au/qcg. Accessed June 11, 2019. 9. Royal Prince Alfred Hospital. Newborn Care Guidelines: Developmental Dysplasia of the Hip. Camperdown, NSW; 2004. https://www.slhd.nsw.gov.au/rpa/neonatal/html/docs/DDHips.pdf. Accessed June 11, 2019. 10. NSW Government. Screening, Assessment and Management of Developmental Dysplasia of the Hip. Clinical Practice Guideline, Resource Manual. Sydney; 2011. http://www.nchn.org.au/docs/Man-DDH.pdf. Accessed June 11, 2019. 11. Safer Care Victoria, Victorian Agency for Health Information. Developmental dysplasia of the hip in neonates | Better Safer Care. https://bettersafercare.vic.gov.au/resources/clinical-guidance/maternity-and-newborn-clinical-network/developmental-dysplasia-of-the-hip-in-neonates#goto-screening. Published 2018. Accessed June 11, 2019. 12. American Academy of Orthopaedic Surgeons. Detection and Nonoperative Management of Pediatric Developmental Dysplasia of the Hip in Infants up to Six Months of Age: Evidence-Based Clinical Practice Guideline.; 2014. https://www.aaos.org/uploadedFiles/PreProduction/Quality/Clinical_Quality_and_Value/Pediatric_Orthopaedics/pediatric-developmental-dysplasia-hip-clinical-practice-guideline.pdf. 13. Patel H. Preventive health care, 2001 update: Screening and management of developmental dysplasia of the hip in newborns. Cmaj. 2001;164(12):1669-1677. 14. Roposch A, Liu LQ, Hefti F, Clarke NMP, Wedge JH. Standardized diagnostic criteria for developmental dysplasia of the hip in early infancy. Clin Orthop Relat Res. 2011;469(12):3451-3461. doi:10.1007/s11999-011-2066-9 15. Jari S, Paton RW, Srinivasan MS. Unilateral limitation of abduction of the hip. A valuable clinical sign for DDH? J Bone Joint Surg Br. 2002;84(1):104-107. 16. Duni A, Ruci V. Reliability of Clinical Tests in developmental dysplasia of the hip. In: Bulletin of the International Scientific Surgical Association. ; 2009:2-3. 17. Fiddian NJ, Gardiner JC. Screening for congenital dislocation of the hip by physiotherapists. Results of a ten-year study. J Bone Jt Surg - Ser B. 1994;76(3):458-459. doi:10.1302/0301-620x.76b3.8175853 18. Choudry Q, Goyal R, Paton RW. Is limitation of hip abduction a useful clinical sign in the diagnosis of developmental dysplasia of the hip? Arch Dis Child. 2013;98(11):862-866. doi:10.1136/archdischild-2012-303121 19. Čustović S, Šadić S, Vujadinović A, et al. The predictive value of the clinical sign of limited hip abduction for developmental dysplasia of the hip (DDH). Med Glas. 2018;15(2):174-178. doi:10.17392/954-18 20. Roposch A, Liu LQ, Protopapa E. Variations in the use of diagnostic criteria for developmental dysplasia of the hip. Clin Orthop Relat Res. 2013;471(6):1946-1954. doi:10.1007/s11999-013-2846-5 21. Şenaran H, Özdemir HM, Ögün TC, Kapicioglu MIS. Value of limited hip abduction in developmental dysplasia of the hip. Pediatr Int. 2004;46(4):456-458. doi:10.1111/j.1442-200x.2004.01931.x 22. Stein-Zamir C, Volovik I, Rishpon S, Sabi R. Developmental dysplasia of the hip: Risk markers, clinical screening and outcome. Pediatr Int. 2008;50(3):341-345. doi:10.1111/j.1442-200X.2008.02575.x 23. Paton RW. Screening in Developmental Dysplasia of the Hip (DDH). Surgeon. 2017;15(5):290-296. doi:10.1016/j.surge.2017.05.002 24. Homer CJ, Baltz RD, Hickson GB, et al. Clinical practice guideline: Early detection of developmental dysplasia of the hip. Pediatrics. 2000;105(4 I):896-905. doi:10.1542/peds.105.4.896 25. Kural B, Devecioğlu Karapınar E, Yılmazbaş P, Eren T, Gökçay G. Risk Factor Assessment and a Ten-Year Experience of DDH Screening in a Well-Child Population. Biomed Res Int. 2019;2019:1-6. doi:10.1155/2019/7213681 26. Talmage MS, Nielson AN, Heflin JA, D’Astous JL, Fedorak GT. Prevalence of Hip Dysplasia and Associated Conditions in Children Treated for Idiopathic Early-onset Scoliosis-Don’t Just Look at the Spine. J Pediatr Orthop. 2020;40(1):e49-e52. doi:10.1097/BPO.0000000000001390 27. Jung HJ, Jang WY, Cho IY, Lee S-H. Hip Screening in Infants Presenting with Asymmetricity of Lower Extremity. J Korean Orthop Assoc. 2017;52(3):205. doi:10.4055/jkoa.2017.52.3.205 28. Paton RW, Choudry Q. Neonatal foot deformities and their relationship to developmental dysplasia of the hip: An 11-year prospective, longitudinal observational study. J Bone Jt Surg - Ser B. 2009;91(5):655-658. doi:10.1302/0301-620X.91B5.22117 29. Paton RW, Choudry QA, Jugdey R, Hughes S. Is congenital talipes equinovarus a risk factor for pathological dysplasia of the hip? A 21-year prospective, longitudinal observational study. Bone Jt J. 2014;96B(11):1553-1555. doi:10.1302/0301-620X.96B11.34130 30. Azzopardi T, Van Essen P, Cundy PJ, Tucker G, Chan A. Late diagnosis of developmental dysplasia of the hip: An analysis of risk factors. J Pediatr Orthop Part B. 2011;20(1):1-7. doi:10.1097/BPB.0b013e3283415927 31. Sharpe P, Mulpuri K, Chan A, Cundy PJ. Differences in risk factors between early and late diagnosed developmental dysplasia of the hip. Arch Dis Child Fetal Neonatal Ed. 2006;91(3):F158-62. doi:10.1136/adc.2004.070870 32. Kliegman R, Stanton B, St. Geme JW, Schor NF, Behrman RE, Preceded by: Nelson WE (Waldo E. The Hip. In: Kliegman R, St. Geme JW, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia: Elsevier; 2019. 33. Kang MS, Han GW, Kam M, Park SS. Clinical significance of asymmetric skin folds in the medial thigh for the infantile screening of developmental dysplasia of the hip. Pediatr Neonatol. 2019;60(5). doi:10.1016/j.pedneo.2019.02.004 34. Anderton MJ, Hastie GR, Paton RW. The positive predictive value of asymmetrical skin creases in the diagnosis of pathological developmental dysplasia of the hip. Bone Jt J. 2018;100B(5):675-679. doi:10.1302/0301-620X.100B5.BJJ-2017-0994.R2 35. Cooke S, Miller D, Gregory J, Roberts A, Kiely N. The Reliability Of Asymmetrical Thigh Creases In The Diagnosis Of Developmental Dysplasia Of The Hip: Is There A Need For Referral To A Paediatric Unit? http://www.priory.com/family_medicine/thigh_dysplasia.htm. Published 2010. Accessed January 10, 2020. 36. Moulder EH, Davies AG. The importance of asymmetric thigh creases as the sole referral complaint in developmental dysplasia of the hip. Orthop Proceedings2. 2018;95-B(Supp_6). https://online.boneandjoint.org.uk/doi/abs/10.1302/1358-992X.95BSUPP_6.BSCOS2012-016. Accessed January 10, 2020. 37. Anderton MJ, Hastie GR, Paton RW. The positive predictive value of asymmetrical skin creases in the diagnosis of pathological developmental dysplasia of the hip. Bone Jt J. 2018;100B(5):675-679. doi:10.1302/0301-620X.100B5.BJJ-2017-0994.R2 38. Barrera CA, Cohen SA, Sankar WN, Ho-Fung VM, Sze RW, Nguyen JC. Imaging of developmental dysplasia of the hip: ultrasound, radiography and magnetic resonance imaging. Pediatr Radiol. 2019;49(12):1652-1668. doi:10.1007/s00247-019-04504-3 |